Single Bundle Anatomic Anterior Cruciate Ligament Reconstruction - Indications, Technique, Results
Annually, over 100,000 anterior cruciate ligament reconstruction procedures happen in the U.S. Although widely accepted and investigated, ACL reconstruction continues to evolve.
Author:Suleman ShahReviewer:Han JuJan 19, 20244.6K Shares70.8K Views
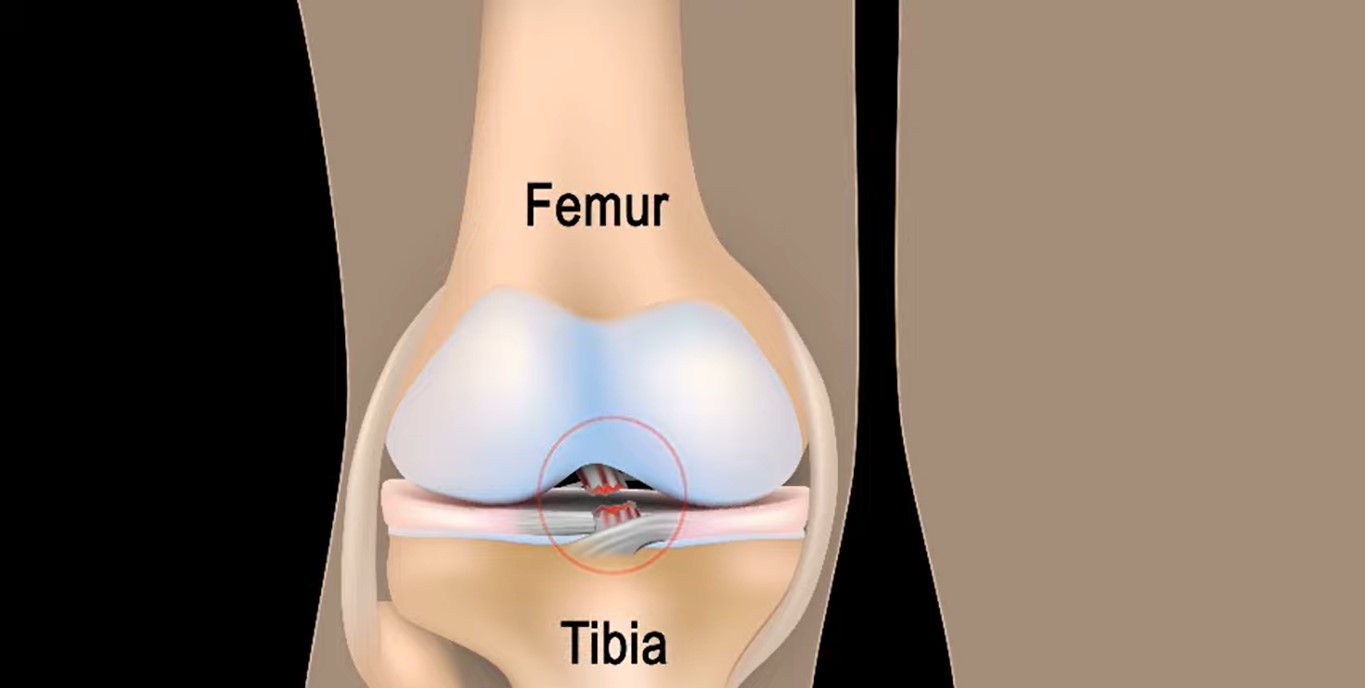
It is widely accepted that anterior cruciate ligament (ACL) reconstruction improves stability and function of the knee and reduces the risk of chondral and meniscal injuries. In ACL-deficient athletes, anterior cruciate ligament reconstruction is the only means of achieving pre-injury level of performance.
However, anterior cruciate ligament reconstruction does not seem to protect the knee from arthrosis, aka osteoarthritis, and conservative treatment can still be indicated in old and inactive patients.
Despite the acknowledgement and the various research works made, anterior cruciate ligament reconstruction still continues to undergo further development, and many technical issues are under debate.
They mainly include:
a. Graft Selection
- patellar tendon
- hamstring
- quadriceps tendon
- allografts
b. Surgical Technique (double versus single bundle)
c. Femoral Tunnel Drilling in Single Bundle Anterior Cruciate Ligament Reconstruction
- transtibial
- antero-medial portal
- outside-in femoral tunnel drilling
The aim of this review was to discuss the indications, techniques, and results of single bundle anatomic anterior cruciate ligament reconstruction.
Indications
After an anterior cruciate ligament tear, three possible treatment options are available:
- conservative treatment
- acute anterior cruciate ligament tear reconstruction (within the first six weeks)
- chronic reconstruction
The following are also needed to be carefully evaluated to correctly plan the treatment:
- patient’s age
- profession
- activity level
As mentioned, anterior cruciate ligament tear reconstruction does not seem to protect the knee from arthrosis in anterior cruciate ligament tear deficient knees. However, a higher incidence of meniscal, chondral, and ligamentous injuries is reported in anterior cruciate ligament tear deficient knees compared to stable knees.
Therefore, sports medicine surgeons have the tendency to indicate anterior cruciate ligament tear reconstruction in young (< 30 years old) and active patients.
Anterior cruciate ligament tear in pediatric patients with open physes needs particular mention.
The treatment of anterior cruciate ligament tears in skeletally immature patients remains controversial, and the debated issues mainly concern the:
- surgical timing (early versus delayed reconstruction)
- most reliable operative technique
Early anterior cruciate ligament tear reconstruction in skeletally immature patients may:
- improve knee function
- avoid strict activity modification in competitive athletes
- reduce progressive chondral and meniscal injuries
However, a wide range of growth disturbances have been reported in animal and clinical studies.
Therefore, conservative management with anterior cruciate ligament tear reconstruction at skeletal maturity should always be mentioned as a possible treatment, most of all, for inactive patients.
Surgery is recommended when:
- the conservative treatment fails (persistent effusion, pain, and recurrent episodes of instability)
- the patient is unwilling or unable to modify the activity level
- meniscal tears amenable to repair are associated with the anterior cruciate ligament tear
Many techniques have been described for pediatric anterior cruciate ligament tear reconstruction, and they include:
- physeal-sparing techniques (intra-articular, extra-articular, and combined intra-/extra-articular)
- partial transphyseal techniques
- complete transphyseal techniques
When anterior cruciate ligament tear reconstruction is indicated in adult patients, graft selection is an important step in pre-operative planning.
Different grafts have been proposed in the literature, and they include:
a. Autografts
- bone-tendon-bone (BTB) or bone-patellar tendon-bone ligament
- hamstrings
- quadriceps tendon
- fascia lata
b. Allografts
- bone patellar-tendon bone ligament/BTB
- hamstrings
- quadriceps tendon
- tibialis anterior or posterior tendon
- Achilles tendon
- fascia lata
- peroneal tendons
c. Synthetic Grafts
- scaffolds
- stents
- prostheses
Although new materials are being investigated, synthetic grafts reported a higher rate of complications compared to autograft and allograft.
Autologous bone patellar-tendon bone (BPTB) and hamstrings as well as allografts are the most commonly used grafts.
Although similar results have been described for these grafts, the authors of this study strongly believe that it is important to individualize the graft choice for each patient’s need.
Surgical Technique
The patient is administered spinal or general anesthesia and positioned supine on the operating table.
A tourniquet is positioned on the proximal thigh. Intravenous antibiotic prophylaxis is performed.
The operative leg is stabilized with an arthroscopic leg holder and the distal extremity of the bed is dropped.
At least 120 degrees of knee flexion needs to be achieved.
A thorough examination under anesthesia is essential to confirm anterior cruciate ligament tear and rule out concomitant ligament injuries.
The tourniquet is inflated after leg elevation.
Graft Harvesting
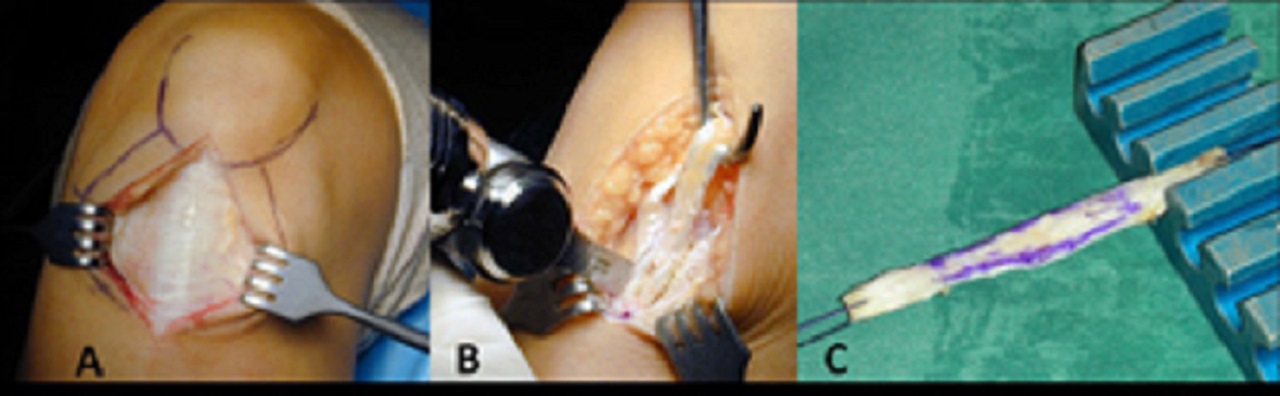
When using a BPTB autograft, a 7 to 8-centimeter anterior/antero-medial incision is performed from the inferior patellar pole to the superior aspect of the tibial tubercle.
The incision is usually slightly medial to the midline of the knee in order to facilitate the tibial tunnel drilling through the same incision.
After incising the paratenon, the central third (around 10 millimeters) of the patellar tendon is harvested with trapezoidal patellar and tibial bone plugs (usually around 9 x 22 millimeters).
Two of No. 2 non-absorbable braided traction sutures are inserted in each plug. The length of the tendon and the bone plugs are measured.
During hamstring harvesting, a 3 to 4-centimeter (cm) longitudinal skin incision is made on the antero-medial aspect of the tibia.
The incision is placed 2 cm medial to the tibial tubercle, started 3 cm below the joint line and prolonged distally.
The sartorial fascia is incised proximally and parallel to the tendons with a No. 15 blade first and then with Metzenbaum scissors.
Deep to the retracted sartorial fascia, the gracilis tendon is visualized proximally and the semitendinosus tendon distally.
The semitendinosus tendon is then pulled out with a blunt hook.
The vinculum to the medial head of the gastrocnemius, and all other minor vincula of the tendon should be released:
- proximally
- distally
- medially
- laterally
When the distal insertion of the tendon is left intact, like in this technique, an open tendon stripper is used.
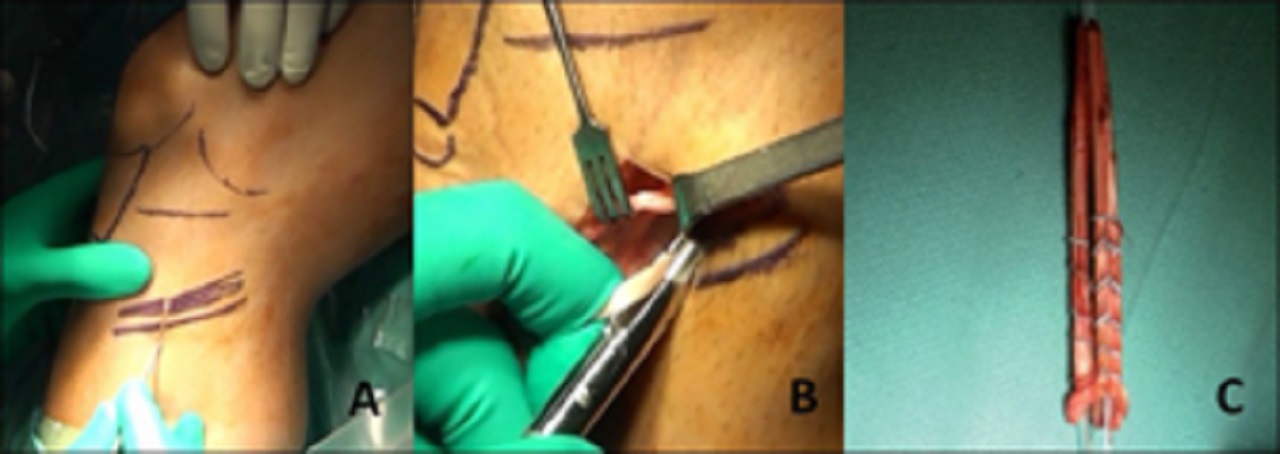
Alternatively, the tendon can be distally detached, armed with a leading suture, and harvested with a closed tendon stripper.
The gracilis tendon is harvested in the same fashion. The tendons are then distally detached and taken to the back table for preparation.
Anterior Cruciate Ligament Reconstruction
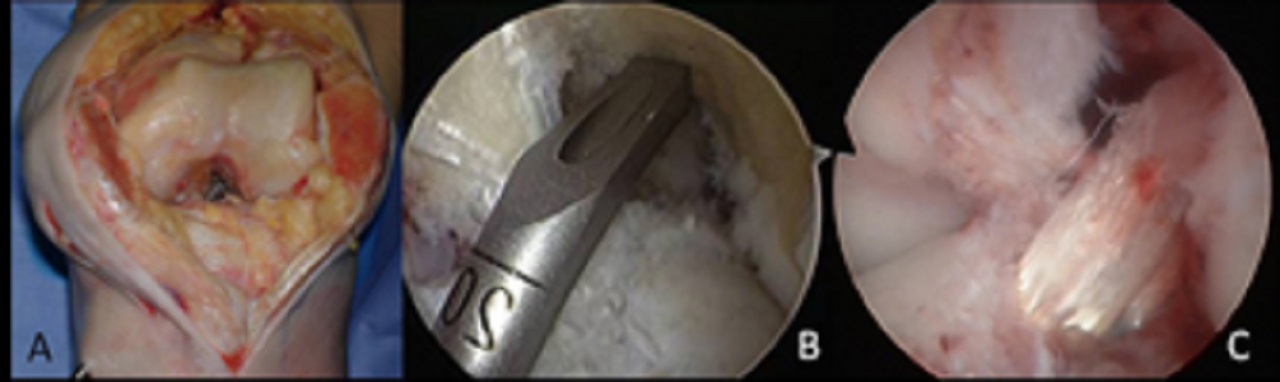
A complete diagnostic arthroscopy is performed through standard anteromedial (AM) and antero-lateral (AL) portals.
Any associated pathologies (meniscal or chondral injuries) are identified and treated at this point.
The remaining anterior cruciate ligament stump is removed with a mechanical shaver until the tibial and femoral footprints are well visualized.
No notchplasty is required, unless osteophytes are visualized in the intercondylar notch.
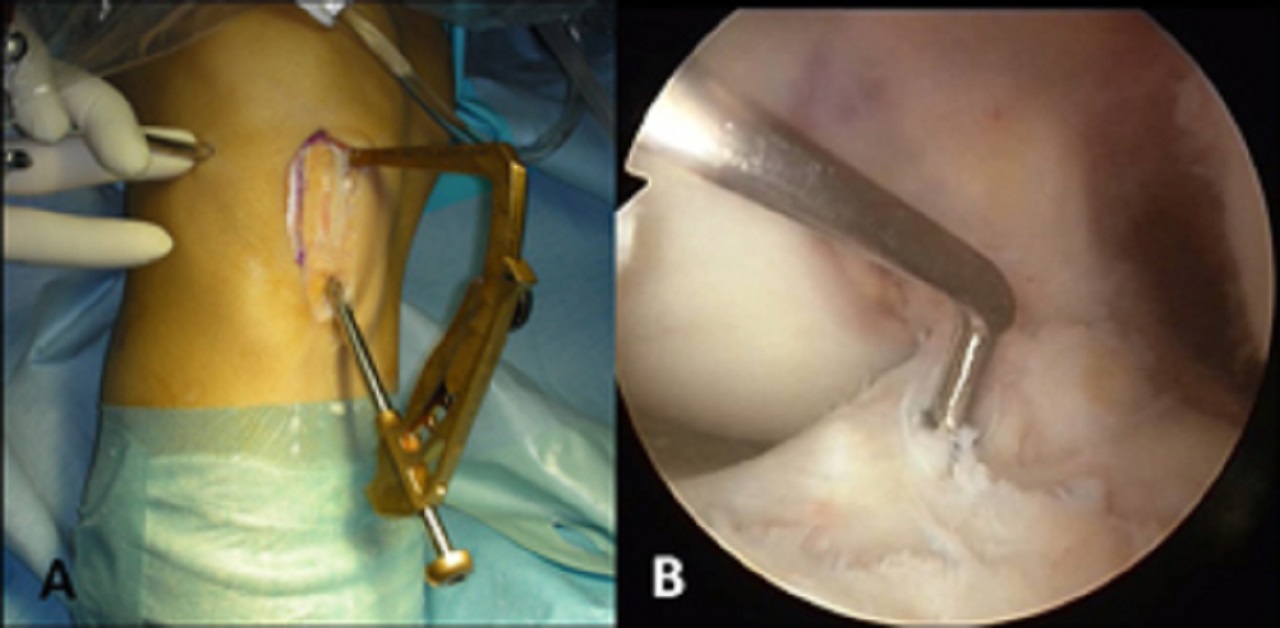
When performing anatomic anterior cruciate ligament reconstruction with AM portal femoral tunnel drilling, either the tibial or the femoral tunnel can be drilled first, according to the surgeon’s preference.
The authors of this study usually prefer to drill the femoral tunnel first.
An arthroscopic offset guide is inserted into the joint through the AM portal.
If the medial wall of the lateral femoral condyle is not adequately visualized through the AL portal, an accessory AM portal can be established to introduce the femoral guide.
Over the top guides are available with different offsets.
The appropriate offset should be decided to preserve a 2-millimeter (mm) posterior wall.
For example, if a 10-millimeter diameter (5 mm radius) femoral tunnel is planned, a 7-millimeter offset guide is used to maintain 2 mm of the posterior wall (7 – 5 = 2 mm).
With the knee at 120-degree flexion, a guide pin is drilled around the 10 o’clock (right knee) position on the coronal plane.
The exit point of the pin through the skin of the lateral thigh should be evaluated.
If the pin is exiting too posterior with respect to the femoral shaft, it should be repositioned to minimize the risk of posterior wall disruption.
A cannulated reamer of the same size of the graft diameter is used to create the femoral tunnel. The femoral tunnel length usually varies from 25 to 30 mm, according to the length of the bone plug or the proximal fixation device.
A No. 2 braided shuttling suture is looped and passed through the eyelet of the guide pin.
The guide pin is pulled from the lateral side of the thigh, retrieving the two free ends of the suture proximally and keeping the loop outside the AM portal.
The free ends are secured with a Kelly clamp.
Then an anterior cruciate ligament tibial guide is inserted into the joint through the AM portal.
Landmarks for the correct positioning of the tibial tunnel are the:
- posterior cruciate ligament (PCL)
- anterior horn of the lateral meniscus
- tibial spines
The anterior cruciate ligament guide is positioned about 7-millimeter:
- anterior to the PCL
- posterior to the anterior horn of the lateral meniscus
- on the lateral wall of the medial tibial spine
When using a BPTB graft, the length of the tibial tunnel is important.
This is determined by:
- measuring the length of the graft; and
- subtracting the femoral bone plug and the intra-articular portion of the graft (usually 30 mm)
A guide pin is drilled into the proximal tibia from a point located halfway between the tibial tubercle and the posteromedial corner of the tibia.
The length of the tibial tunnel can be measured with the guide pin. A cannulated reamer with the same diameter of the graft is used to drill the tibial tunnel.
An arthroscopic grasper is inserted into the tibial tunnel and the loop of the suture, previously positioned in the femoral tunnel, is then retrieved out of the tibial tunnel distal aperture.
The graft is then inserted into the joint and fixed.
Fixation Of The Graft And Postoperative Rehabilitation
The preferred fixation of the authors of this study for the anterior cruciate ligament is as follows:
- When using a BPTB graft, fixation is achieved with two interference screws on both the femoral (first) and tibial sides.
- When using a soft tissue autograft or allograft, fixation is achieved proximally with an extracortical flip button device and distally with an interference screw.
Discussion
Autograft VS. Allograft
During the decision-making process regarding a patient undergoing anterior cruciate ligament reconstruction, the first step is defining the type of graft.
The use of autograft (mostly BPTB and hamstring) is widely accepted.
The use of readily available allografts has recently grown in popularity, in order to reduce donor-site morbidity and expedite post-operative rehabilitation compared to autografts.
However, some tissue banks irradiated or chemically treated the grafts as a means of sterilization or preservation. This led to inferior outcomes of allograft anterior cruciate ligament reconstruction compared to autograft.
Although sterilization and preservation have considerably improved over the years, tissue-processing techniques are not currently standardized yet.
Potential disadvantages of allograft tissue include disease transmission, autoimmune response, delayed or incomplete biological incorporation and increased costs.
In a recent systematic review, the authors compared the results of anterior cruciate ligament reconstruction with autografts and non-irradiated, non-chemically treated allografts.
The authors found that no statistically significant differences existed between autografts and non-chemically processed non-irradiated allografts in:
- Lysholm scores
- International Knee Documentation Committee (IKDC) scores
- Lachman examinations
- pivot-shift testing
- KT-1000 measurements
- failure rates
However, the authors of this study included only 11 papers in their systematic review and warn the readers that further large-scale, well-designed studies are required to confirm these findings.
In another meta-analysis of 5,182 patients, the authors compared the results of BPTB autograft versus allograft in anterior cruciate ligament reconstruction.
Data from both fresh-frozen and irradiated allografts were used.
They found that outcomes on subjective IKDC, Lysholm, Tegner, single-legged hop, and KT-1000 arthrometer were significantly better in autografts.
Alternatively, return to pre-injury level, overall IKDC, pivot shift and anterior knee pain were significantly in favor of allografts.
Allograft BPTB demonstrated a three-fold increase in rerupture rates compared to autograft (12.7% and 4.3%, respectively).
The authors concluded that patients undergoing anterior cruciate ligament reconstruction with autologous BPTB grafts demonstrated:
- lower rates of graft rupture
- lower levels of knee laxity
- improved single-legged hop test results
Also, in general, those patients were more satisfied than the patients who received allograft BPTB reconstruction.
Considering the long-term follow-up and larger case series with autografts, the authors strongly believe that autologous BPTB and hamstring grafts still represent the gold standard in anterior cruciate ligament reconstruction.
Allograft is a valuable alternative option in selected cases.
Bone-Patellar Tendon-Bone VS. Hamstring
Controversy also exists regarding the outcomes of BPTB and HS autografts.
In a review published in 2011 by Cochrane Database of Systematic Reviews, the authors, with Nicholas G. H. Mohtadi as lead author, included randomized and quasi-randomized controlled trials comparing outcomes (minimum two-year follow-up) following anterior cruciate ligament reconstruction using either BPTB or hamstring autografts in skeletally mature adults, irrespective of the:
- number of bundles,
- fixation method; or
- incision technique
The authors of this study found that pooled data for primary outcomes showed no statistically significant differences between the two graft choices for:
- functional assessment (single leg hop test)
- return to activity
- Tegner and Lysholm scores
- subjective measures of outcome
There were also no differences for rerupture or IKDC scores.
All tests (instrumental, Lachman, pivot shift) for static stability consistently showed that BPTB reconstruction resulted in a more statically stable knee compared to hamstring.
However, patients experienced more anterior knee problems, especially with kneeling, after BPTB reconstruction.
BPTB reconstructions resulted in a statistically significant loss of extension range of motion.
Alternatively, hamstring reconstructions demonstrated a trend towards loss of flexion range of motion and a statistically significant loss of knee flexion strength.
The clinical importance of the range of motion losses is still unclear.
In the light of these findings, the authors believe that BPTB and hamstring autografts are equally valuable options in anterior cruciate ligament reconstruction.
- needs
- profession
- activity level
- age
- choice of sports
Anteromedial Portal VS. Transtibial Femoral Tunnel Drilling
Traditionally, the femoral tunnel has been drilled through the tibial tunnel (transtibial technique).
However, this procedure poses the risk of a high/vertical placement of the femoral tunnel in the intercondylar notch and a posterior tibial tunnel placement on the plateau.
This usually results in a non-anatomic anterior cruciate ligament reconstruction.
The transtibial technique achieves good-to-excellent results in only 60% of patients, and 20% to 30% of athletes do not regain their previous level of performance.
For these reasons, surgeons started creating two independent tunnels, by drilling the femoral tunnel from the antero-medial portal (Antero-medial portal technique).
In this fashion, the surgeon can place the tunnels anatomically and with more freedom compared to the transtibial technique.
Antero-medial portal technique allows for anatomical tunnel placement and improved knee biomechanics.
However, in a recent retrospective study carried out from the data of the Danish Knee Ligament Reconstruction Register, an increased risk of revision after antero-medial compared with transtibial technique during primary anterior cruciate ligament reconstruction has been described.
The authors of this study stated that their findings could be explained:
- by technical failures resulting from introduction of a new and more complex procedure; or
- by the hypothesis that, compared to non-anatomic techniques, a greater force is carried by the anatomic anterior cruciate ligament reconstruction
Hence, there is a concomitant higher risk of anterior cruciate ligament rupture.
According to the data presented and their clinical experience, the authors believe that a sports medicine surgeon should consider both the techniques.
However, antero-medial portal technique allows for more anatomic tunnel positioning and better biomechanical results compared to transtibial technique.
Single VS. Double Bundle ACL Reconstruction
Another controversy regarding anterior cruciate ligament reconstruction is about single versus double-bundle reconstruction.
The double-bundle technique, popularized by orthopedic surgeon Dr. Freddie H. Fu (1950-2021), was developed from a good understanding of the native anterior cruciate ligament anatomy and its two functionally different bundles (antero-medial and posterolateral).
The double-bundle technique allows for both bundle reconstruction through four different tunnels.
In a recent meta-analysis, double-bundle technique apparently resulted in significantly better anterior and rotational stability and higher IKDC objective scores compared to single-bundle reconstruction.
However, the meta-analysis did not detect any significant differences in subjective outcome measures between double-bundle and single-bundle reconstruction, as evidenced by the:
- Lysholm score
- Tegner activity scale
- IKDC subjective score
Alternatively, in a recent Cochrane review, the authors stated that there is insufficient evidence to determine the relative effectiveness of double-bundle and single-bundle anterior cruciate ligament reconstruction in adults.
However, the authors found limited evidence that double-bundle anterior cruciate ligament reconstruction has some superior results in objective measurements of knee stability and protection against:
- repeat anterior cruciate ligament rupture, or
- a new meniscal injury
Conversely, a meta-analysis regarding in vitro and intraoperative laxities after single-bundle and double-bundle anterior cruciate ligament reconstructions demonstrated that both techniques result in similar antero-posterior knee joint laxity at time 0.
Therefore, no conclusive evidence on the superiority of one reconstruction technique over the other in terms of rotation laxity could be obtained.
In the light of these data, the authors do not commonly perform double-bundle anterior cruciate ligament reconstruction due to the more complex and expensive surgical technique.
Conclusion
Anterior cruciate ligament reconstruction is a common procedure in orthopedic surgery.
However, this surgery needs to be done by experienced surgeons, with experience in many different reconstruction techniques.
To achieve good results and high satisfaction rates, correct treatment must be tailored to meet the patient’s needs, profession, activity level, age, and sports.
Considering the literature review, many controversies regarding anterior cruciate ligament reconstruction are still under debate and need to be clarified with high quality studies.

Suleman Shah
Author
Suleman Shah is a researcher and freelance writer. As a researcher, he has worked with MNS University of Agriculture, Multan (Pakistan) and Texas A & M University (USA). He regularly writes science articles and blogs for science news website immersse.com and open access publishers OA Publishing London and Scientific Times. He loves to keep himself updated on scientific developments and convert these developments into everyday language to update the readers about the developments in the scientific era. His primary research focus is Plant sciences, and he contributed to this field by publishing his research in scientific journals and presenting his work at many Conferences.
Shah graduated from the University of Agriculture Faisalabad (Pakistan) and started his professional carrier with Jaffer Agro Services and later with the Agriculture Department of the Government of Pakistan. His research interest compelled and attracted him to proceed with his carrier in Plant sciences research. So, he started his Ph.D. in Soil Science at MNS University of Agriculture Multan (Pakistan). Later, he started working as a visiting scholar with Texas A&M University (USA).
Shah’s experience with big Open Excess publishers like Springers, Frontiers, MDPI, etc., testified to his belief in Open Access as a barrier-removing mechanism between researchers and the readers of their research. Shah believes that Open Access is revolutionizing the publication process and benefitting research in all fields.

Han Ju
Reviewer
Hello! I'm Han Ju, the heart behind World Wide Journals. My life is a unique tapestry woven from the threads of news, spirituality, and science, enriched by melodies from my guitar. Raised amidst tales of the ancient and the arcane, I developed a keen eye for the stories that truly matter. Through my work, I seek to bridge the seen with the unseen, marrying the rigor of science with the depth of spirituality.
Each article at World Wide Journals is a piece of this ongoing quest, blending analysis with personal reflection. Whether exploring quantum frontiers or strumming chords under the stars, my aim is to inspire and provoke thought, inviting you into a world where every discovery is a note in the grand symphony of existence.
Welcome aboard this journey of insight and exploration, where curiosity leads and music guides.
Latest Articles
Popular Articles