Pulmonary Edema - Mechanisms And Treatment In COVID-19 Patients
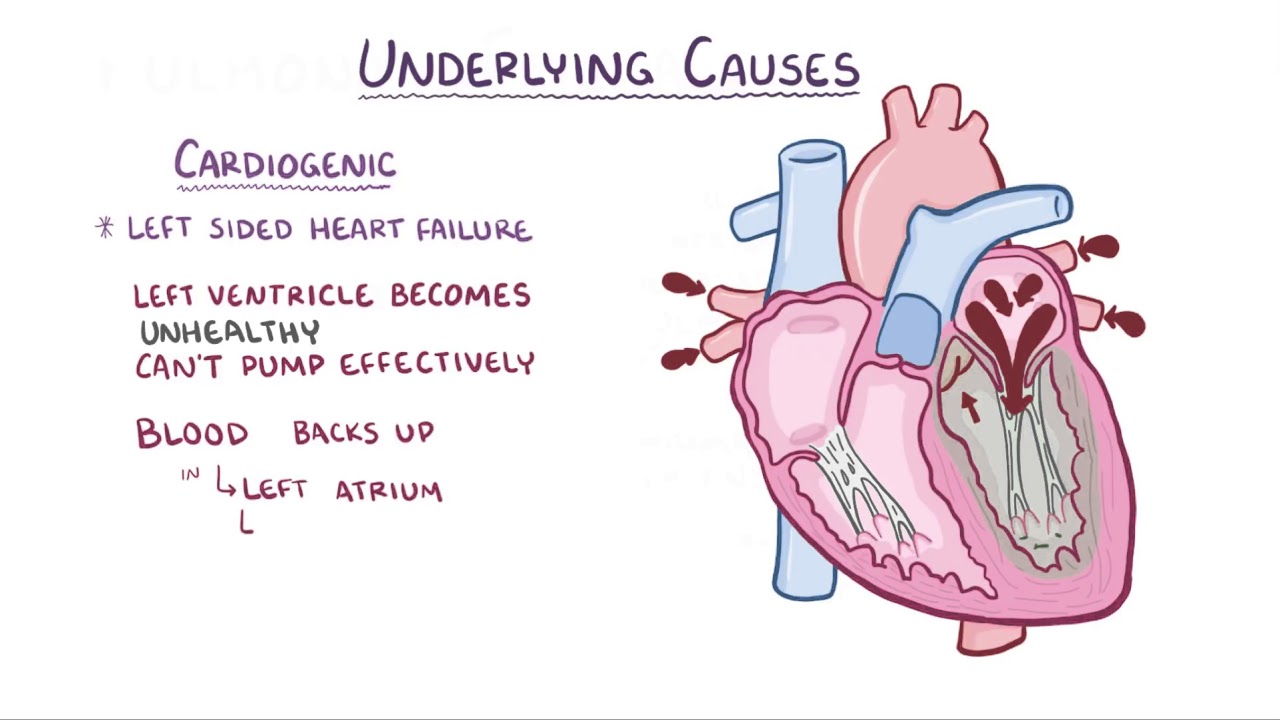
Pulmonary edema is caused by an imbalance between the way lung tissue fluid is made and how it flows back out of the lungs. This leads to a large amount of tissue fluid being absorbed by the lungs' lymph and veins. The fluid leaks into the interstitial space of the lungs and builds up there.
Author:Suleman ShahReviewer:Han JuAug 04, 202213 Shares583 Views

Pulmonary edemais caused by an imbalance between the way lung tissue fluid is made and how it flows back out of the lungs. This leads to a large amount of tissue fluid being absorbed by the lungs' lymph and veins.
The fluid leaks into the interstitial space of the lungs and builds up there. Eventually, it gets into the alveoli, which are the air sacs in the lungs. This causes severe problems with pulmonary ventilation and gas exchange.
Pulmonary edema can be found in COVID-19 patients with a lung ultrasound and a computerized tomography (CT) scan.
The condition looks like a slow-developing pneumonia with interstitial pulmonary edema that gets worse quickly in the late stages and alveolar edema that gets worse slowly at first.
At the moment, these are the main effects of a pulmonary virus infection. It is known that SARS-CoV-2 gets into human cells by attaching to ACE-2 receptors and other membrane ectopeptidases.
When it gets to the lungs, the virus and virus-mediated interactions between proteins cause an inflammatory storm in the lungs. This is what causes the increasing vascular permeability in the lungs and pulmonary edema.
Virological Characteristics Of COVID-19
SARS-CoV-2 is the seventh coronavirus that can infect humans. It is an enveloped RNA coronavirus of the genus β. Coronavirus has glycoproteins, membranes, and nucleic acids as part of its structure.
The spike (S) protein of coronavirus, which is one of the surface glycoproteins, is made up of two functional units called S1 and S2. By binding to host receptors, S1 makes it easier for the virus to get into the host cell, and S2 controls membrane fusion to let viral RNA get into the host cell so it can continue to replicate.
So, the S protein tells the virus which cell it will infect, controls how the virus attaches to and fuses with the host cell membrane, and encourages cell invasion. Because of this, the S protein is necessary for viruses to spread.
It has been shown that SARS-CoV-2 infects human cells by the specific binding of S-protein to angiotensin-converting enzyme 2 (ACE2), and the binding affinity between these two proteins is 10–20 times greater than that of SARS-CoV and ACE2. Human vascular endothelial cells, alveolar epithelial cells, and intestinal epithelial cells all have a lot of ACE2 in them.
It is also highly expressed in cardiomyocytes, epithelial cells of the proximal convoluted tubule of the kidney, urothelial cells, the esophagus, and the ileum. This makes it easier for SARS-COV-2 to get into the human body and cause problems.
Pulmonary Edema - causes, symptoms, diagnosis, treatment, pathology
Abnormal Lung Humoral Metabolism In COVID-19
When SARS-CoV-2 gets into the body, it damages alveolar and vascular epithelial cells. This causes a small clot to form, which raises pulmonary vein pressure and vascular permeability and causes a lot of tissue fluid to leak out.
In addition to these direct causes of COVID-19 pulmonary edema, there are other factors that can affect the AFC and PFC and cause pulmonary edema. These factors can be thought of as having an abnormal humoral metabolism.
The main sign of an abnormal humoral metabolism is an imbalance of water and electrolytes. Most people have problems with water and sodium, and their serum potassium levels are also often off. It has been shown that how often and how bad COVID-19 is is closely linked to how inorganic salts are broken down in the body.
CODIV-19 tends to get worse as serum sodium goes down. Hyponatremia, which means that there isn't enough sodium in the blood, and low potassium and calcium levels in the blood serum are also linked to COVID-19.
In COVID-19 patients, pulmonary edema can be caused by the functional inhibition of important enzymes and ion channels in the lungs. AFC is controlled by Na+/K+-ATPase and ion channels (sodium, potassium, AQPs, and TRPs).
Conventional Treatment Of Pulmonary Edema In COVID-19 Patients
At the moment, there are many clinical trials going on to test coronavirus treatments, such as new drugs and drugs that have been repurposed or repositioned. As COVID-19 treatments for people with severe infections, immune-modulating drugs, supportive care, and antiviral drugs have all been tried.
Tocilizumab, human immunoglobulin, and convalescent plasma are immune-modulating drugs that can be used for COVID-19.
It was thought that the IL6 monoclonal antibody, also known as tocilizumab, worked by calming the inflammatory storm that followed an infection. However, the most recent clinical study published in NEJM showed that tocilizumab did not prevent intubation or death in mild COVID-19 patients who were hospitalized.
Convalescent plasma was first shown to help COVID-19 patients with severe infections by stabilizing their immune systems. The next randomized controlled trial, on the other hand, didn't show any major changes in 28 days.
Supportive care for COVID-19 includes help with breathing and blood flow. Patients get a high-flow nasal cannula (HFNC), non-invasive ventilation (NIV), mechanical ventilation, or extracorporeal membrane oxygenation (ECMO) to help them breathe.
They also get a crystalloid fluid to keep their body fluids in balance and anticoagulants to stop clots from forming to help their circulation. These helpful approaches have been shown to help COVID-19 patients as part of their treatment.
Drugs that have been shown to work against viruses have been used to treat other viral infections. But it's not clear if these drugs work and are safe for COVID-19 patients. So far, the FDA has only approved remdesivir for compassionate use in COVID-19 patients who are very sick.
In randomized, placebo-controlled trials with COVID-19 patients, other antiviral drugs like arbidol, chloroquine phosphate, and ritonavir did not work. Even so, it seems reasonable that antiviral therapycould be given to people at high risk as soon as possible instead of waiting for the disease to get worse.
Other therapies, like organ support, glucocorticoid therapy, and nutritional support, have been used in the clinical treatment of COVID-19, but not much is known about how well they work. But in all of the above treatments, not much attention has been paid to the abnormal humoral metabolism and pulmonary edema, which are two of the main things that put patients' lives at risk.
Putative Drug Targets For Pulmonary Edema In COVID-19 Patients
Pulmonary edema is caused by things like ion channels, AQPs, RAS, bradykinin, and hyaluronic acid. The main things that put COVID-19 patients at risk of dying are their abnormal humoral metabolism and the pulmonary edema that results from it.
So, one of the most important parts of treating COVID-19 patients should be getting rid of the pulmonary edema. Since this is the case, drugs that can normalize humoral metabolism should be tested in the clinic to see if they can help COVID-19 patients.
Pulmonary Edema causes, symptoms, diagnosis, treatment, pathology
Targeting Potassium Channels
ENaC's expression is changed by potassium channels. It has been said that K+ channel openers can turn on transepithelial ion transport in alveolar monolayers under physiological conditions in the lab.
KCa3.1 (1-EBIO) and KATP (minoxidil) channel openers can greatly improve AFC in mice given verapamil, which is a calcium channel antagonist from the first generation of the phenylalkylamine class. This suggests that K+ channel openers could be used to treat pulmonary edema.
Targeting Aquaporins And Transient Receptor Potential Ion Channels
AQP-5 plays a big role in pulmonary edema, and AQP-5 expression has been seen to go down as the disease gets worse. By making AQP-1 and AQP-5 more active in rats with acute lung damage caused by LPS, dexmedetomidine can cause pulmonary edema.
Lipoxin A4 (LXA4) can stop alveolar fluid from leaking out by stabilizing the permeability of pulmonary microvascular endothelial cells by controlling the expression of AQP-5 and MMP-9. TRPA1, TRPV1, and TRPV4 are the most important TRPs for the respiratory system and pulmonary edema.
Stopping these TRPs from working could help treat pulmonary edema. In a recent review, the effects of TRPs on chemical injuries to the lungs were summed up. This review looked at TRPA1, TRPV1, and TRPV4 antagonists that have been studied both in the lab and in people.
Renin-Angiotensin System And Bradykinin Targeting
The RAS is a very important part of both ARDS and pulmonary edema. The things that the molecules in the RAS do are controlled by changes that happen in response to an injury. AT1 receptor activation makes pulmonary edema worse, so drugs that block AT1 receptors, like losartan and valsartan, may be able to reduce pulmonary edema.
However, early reports showed that some ACE inhibitors and ARBs don't help much in treating COVID-19, while othershelp protect patients with high blood pressure who already have it. It was said that patients with high blood pressure who took ARBs had a 76% lower chance of getting COVID-19.
Also, it was shown that giving Ang (1–7) from outside the body helped reduce inflammationand improve pulmonary function in ARDS models. In the clinical study of ARDS, recombinant ACE2 was also said to be a possible therapy. This is because it can quickly lower the level of Ang II in the blood and the expression of IL-6.
Natural Compounds And Traditional Chinese Medicines For The Treatment Of Pulmonary Edema In COVID-19
In addition to the chemical drugs and compounds we talked about above, natural compounds and traditional Chinese medicines (TCM) also have antiviral effects against SARS-CoV-2 and have made important contributions to curing COVID-19, especially by reducing pulmonary edema and stopping the disease from getting worse.
TCM says that the bad things about COVID-19 come from cold-dampness, which is caused by "toxin" and "dampness." "Toxin" refers to pathogenic microorganisms and inflammatory substances that are present in infected patients. "Dampness" refers to an abnormal humoral metabolism, such as inflammatory exudation.
Here, we've summed up a few natural compounds and TCM formulas that are likely to be used as drugs in the future or that have already worked well for COVID-19 patients.
Natural Compounds And Their Effects On Syndrome Coronavirus 2 Infections
A lot of research has been done to find natural compounds that fight viruses and reduce pulmonary edema. Some of these compounds have already been tested against SARS-CoV and SARS-COV-2.
Natural compounds can stop the virus from attaching itself to the ACE2 receptor on the host cell. Cepharanthine is a bisbenzylisoquinoline alkaloid made from the tubers of Stephania Japonica. It was found to stop the spread of pan-β-coronavirus in a wide range of cells.
In the study of SARS-CoV, emodin, which is an anthraquinone compound from the genera Rheum and Polygonum, can stop the binding of S protein and ACE2 by a large amount. RNA-dependent RNA polymerase (RdRp) is an important protease that speeds up the process of making copies of RNA from RNA templates. This makes it an attractive therapeutic target.
When Theaflavin from black tea docks in the catalytic pocket of SARS-CoV-2 RdRp, it has a lower binding energy. So, it might be able to stop SARS-CoV-2 from making RdRp.
Pulmonary edema can be helped by stopping the inflammatory storm. Atractylenolide-I, the active component of atractylodes, may reduce the production of IL-6 and TNF-α by inhibiting the production of inflammatory cytokines that cause an inflammatory response. This would make it less likely that pulmonary edema would happen.
Traditional Chinese Medicines And COVID-19 Infection
In China, COVID-19 has already been treated with a number of TCMs, and there has been a high rate of recovery. Lian-Hua-Qing-Wen capsules change the shape of viruses in a big way, stop SARS-CoV-2 from replicating with an IC50 of 411.2 μg/ml, reduce the production of pro-inflammatory cytokines at the mRNA level, and have an anti-inflammatory effect in vitro.
It has been found that COVID-19 patients who took Lian-Hua-Qing-Wen capsules for 14 days had a much higher recovery rate of 91.5 percent and a median time to symptom recovery of 7 days, which was much shorter than the control group, which used standard treatment. The ingredient ephedra can also cause bronchodilation, help people with breathing problems, and reduce pulmonary edema.
By regulating the PaO2/FiO2 and ROX index, the toad venom injection can improve the pulmonary function of COVID-19 patients by a lot. This makes pulmonary edema go away. As reported, the PaO2/FiO2 index and ROX index of patients who got standard treatment plus 20 ml of toad venom per day improved by a lot (from 111.30 to 35.90 for PaO2/FiO2 and from 7.56 to 2.94).
The number of people in the treatment group whose PaO2/FiO2 and ROX index were better than those in the control group was higher (95.2% vs. 68.4% and 73.7%). Also, after a week of treatment, the peripheral blood mononuclear lymphocytes of COVID-19 patients were much better. They went from 0.91 ± 0.54 to 1.24 ± 0.67, while the control group didn't change much.
The pharmacodynamic component of the Liu Shen capsule is also toad venom, and it has been shown to have antiviral and anti-inflammatory effects on SARS-CoV-2 in the lab. It can stop the virus from replicating in Vero E6 cells, reduce the production of inflammatory cytokines at the mRNA level, and block the NF-B signaling pathway to turn down the expression of cytokines.
People Also Ask
What Happens During A Pulmonary Edema?
When fluid builds up in the lungs' air sacs, or alveoli, it causes pulmonary edema, making breathing harder. This may result in respiratory failure and interfere with gas exchange.
Is Pulmonary Edema Life Threatening?
A hazardous medical disease called pulmonary edema is brought on by too much fluid in the lungs' alveoli. Even though it can be caused by conditions other than heart disease, heart disease is the most common cause.
How Long Can You Survive With Pulmonary Edema?
In-hospital mortality among patients who required mechanical breathing was 55% (12/22 cases). Mortality in hospitals was 12% in 18 patients. The average time between the start of pulmonary oedema and death was 5 days (between 1 and 40 days).
Is Pneumonia And Pulmonary Edema The Same?
While pulmonary edema and pneumonia both result in a kind of lung accumulation, the former is typically brought on by CHF. On the other hand, infection is what causes pneumonia. If your immune system is already weak, getting a cold or the flu more often could make you more likely to get pneumonia.
Conclusion
The severity of the symptoms and mortality of COVID-19 patients are attributed in part to the aberrant humoral metabolism and pulmonary edema.
ARDS and pulmonary edema are caused by decreased alveolar Na-K-ATPase expression, abnormal bradykinin and hyaluronic acid metabolism, dysregulation of sodium and potassium channels, aquaporins, and the renin-angiotensin system, as well as a cytokine inflammatory storm.
This in turn causes COVID-19 patients to suffer serious lung damage. Further research should be done on existing medications and inhibitors that target the elements of humoral metabolism as possible COVID-19 therapies. Also, research on the effectiveness and safety of natural substances and TCMs, which often have many targets, is necessary.
In COVID-19 patients, concentrating on reducing the development of body fluid in the lung or encouraging body fluid absorption may help reduce lung damage and death. Drugs that target humoral pathways may thus prove to be very successful against SARS-CoV-2 infections.
Jump to
Virological Characteristics Of COVID-19
Abnormal Lung Humoral Metabolism In COVID-19
Conventional Treatment Of Pulmonary Edema In COVID-19 Patients
Putative Drug Targets For Pulmonary Edema In COVID-19 Patients
Natural Compounds And Traditional Chinese Medicines For The Treatment Of Pulmonary Edema In COVID-19
People Also Ask
Conclusion

Suleman Shah
Author
Suleman Shah is a researcher and freelance writer. As a researcher, he has worked with MNS University of Agriculture, Multan (Pakistan) and Texas A & M University (USA). He regularly writes science articles and blogs for science news website immersse.com and open access publishers OA Publishing London and Scientific Times. He loves to keep himself updated on scientific developments and convert these developments into everyday language to update the readers about the developments in the scientific era. His primary research focus is Plant sciences, and he contributed to this field by publishing his research in scientific journals and presenting his work at many Conferences.
Shah graduated from the University of Agriculture Faisalabad (Pakistan) and started his professional carrier with Jaffer Agro Services and later with the Agriculture Department of the Government of Pakistan. His research interest compelled and attracted him to proceed with his carrier in Plant sciences research. So, he started his Ph.D. in Soil Science at MNS University of Agriculture Multan (Pakistan). Later, he started working as a visiting scholar with Texas A&M University (USA).
Shah’s experience with big Open Excess publishers like Springers, Frontiers, MDPI, etc., testified to his belief in Open Access as a barrier-removing mechanism between researchers and the readers of their research. Shah believes that Open Access is revolutionizing the publication process and benefitting research in all fields.

Han Ju
Reviewer
Hello! I'm Han Ju, the heart behind World Wide Journals. My life is a unique tapestry woven from the threads of news, spirituality, and science, enriched by melodies from my guitar. Raised amidst tales of the ancient and the arcane, I developed a keen eye for the stories that truly matter. Through my work, I seek to bridge the seen with the unseen, marrying the rigor of science with the depth of spirituality.
Each article at World Wide Journals is a piece of this ongoing quest, blending analysis with personal reflection. Whether exploring quantum frontiers or strumming chords under the stars, my aim is to inspire and provoke thought, inviting you into a world where every discovery is a note in the grand symphony of existence.
Welcome aboard this journey of insight and exploration, where curiosity leads and music guides.
Latest Articles
Popular Articles
